Comments from the Expert Advisory Committee
- Lyme disease (Lyme borreliosis) is an infection caused by Borrelia bacteria and is spread through the bite of an infected tick to a person.

- Lyme disease can affect anyone but is most common amongst those who spend time in grassy or heavily wooded areas or are in contact with certain animals e.g. deer and sheep. Most cases occur in the summer and autumn.
- Only a small number of individuals will develop Lyme disease following a tick bite. However, early identification of Lyme disease with prompt and appropriate antibiotic therapy is important to minimise the likelihood of the development of late stage infection and/or long term complications of Lyme disease.
- Lyme disease from an infected tick bite can be prevented if the tick is removed within 24 to 36 hours. If tick remains on the skin, carefully remove it as soon as possible. Link to instructions.
- Testing of removed ticks is not recommended as the presence of Borrelia is not a reliable predictor of the development of infection in humans.
- Symptoms of Lyme disease may take months or years to resolve even after treatment for several reasons, including alternative diagnoses, reinfection, treatment failure, immune reaction, and organ damage caused by Lyme disease.
Diagnosis of Lyme Disease
Early localised disease (erythema migrans)
- Erythema migrans should be diagnosed and treated without laboratory testing as antibodies to Borrelia bacteria take several weeks to develop. Serological testing is not indicated before or after antibiotic treatment of erythema migrans.
- Early localised disease is a clinical diagnosis:
- Assess for tick exposure risk
- More than two-thirds of tick bites in adults involve the limbs; more than three-quarters of tick bites in children involve the head and neck.
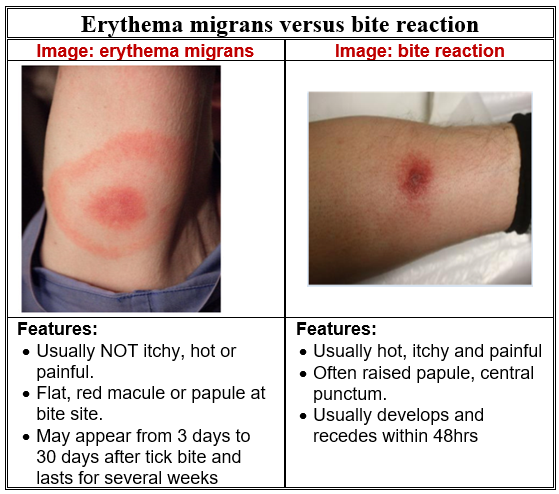
- Erythema migrans may present as a ‘bulls-eye’ skin rash in 70% of adults and 50% of children. It is not usually itchy, hot or painful but increases in size and may sometimes have a central clearing.
- Rash usually develops between 3 to 30 days after a tick bite and lasts for several weeks at site of tick bite.
- Patients may also complain of influenza-like symptoms such as headache, sore throat, neck stiffness, fever, muscle aches and general fatigue.
- Visit Health Protection Surveillance Centre Diagnostic Support Tool
- Be aware that a rash that is not erythema migrans can develop as a reaction to a tick bite. This rash usually develops and recedes within 48 hours from the time of the tick bite.
Early Disseminated Disease and Later Stage Infection
- Use a combination of clinical presentation and serological testing in patients with early disseminated disease or later stage infection.
- Clinical presentation may include:
- Severe flu-like illness, musculoskeletal, neurological, cutaneous or cardiac symptoms
- Discuss case with Microbiology/ID specialist including the urgency of specialist review and advice on antibiotic therapy.
- Antibodies to Borrelia are usually detectable within 4-8 weeks of infection. Patients with late-stage infection are rarely seronegative and usually have very strongly positive antibody tests.
- Testing for Lyme disease should only be performed by an accredited laboratory that use validated tests and participate in a formal external quality assurance programme.
- The occurrence of false-positive tests in patients with other infections or conditions such as autoimmune diseases, can lead to misdiagnosis and inappropriate treatment. Other specialised investigations may be necessary for confirmation of a positive result.
- Visit HPSC website for further information
Treatment
When to treat:
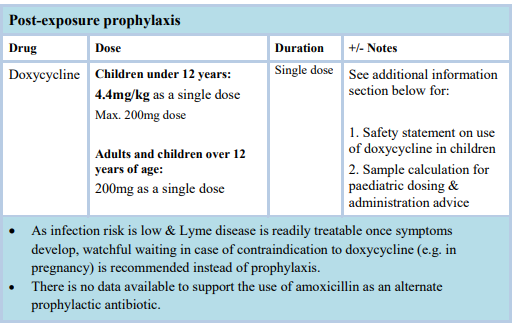
- The risk of Lyme disease is very low if a tick has been attached less than 36 hours. If a tick has been attached for greater than 36 hours or if it is not possible to ascertain duration of tick attachment post-exposure prophylaxis may be considered.
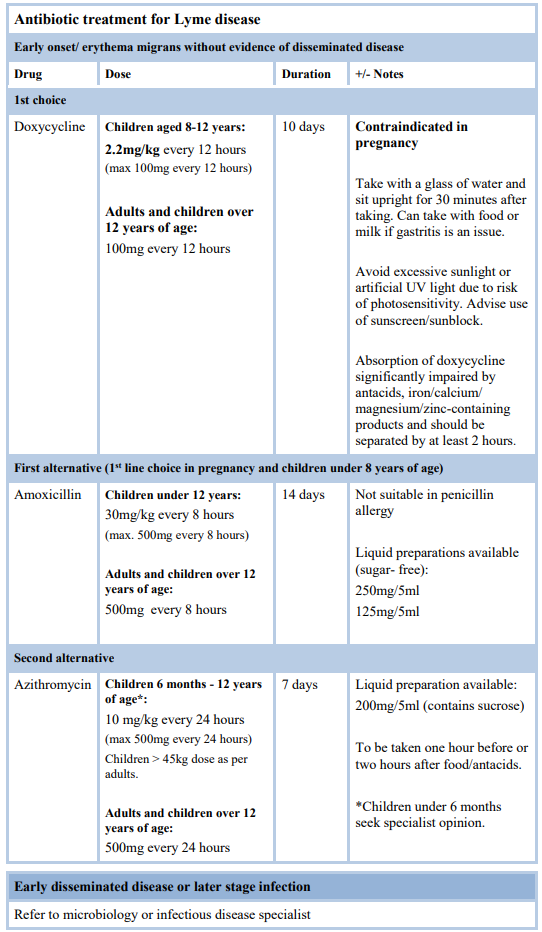
- All patients symptomatic of Lyme disease should be treated with appropriate antibiotics.
- Appropriate antibiotics minimise the likelihood of the development of late stage infection and long-term complications of Lyme disease through a) post-exposure prophylaxis or b) early treatment of erythema migrans.
- Antibiotics are not recommended where Lyme disease has previously been adequately treated (post-Lyme disease syndrome) – there is no demonstrable clinical benefit from prolonged antibiotic therapy and the risk of harm outweighs the benefit. Supportive management should be offered (e.g. management of chronic pain, fatigue, depression, sleep disturbance). Seek specialist advice if necessary.
- Some people may experience a Jarisch-Herxheimer reaction in response to antibiotic treatment of Lyme disease. It is an acute febrile illness which can cause an exacerbation of symptoms (fever, chills, muscle pain, headache). The reaction is self-limiting, usually resolving within 24 to 48 hours and does not usually warrant stopping treatment.
Additional information
Safety statement on the use of doxycycline in children under 8 years of age
- Patients and prescribers should be aware that the use of doxycycline in children under 8 years of age is unlicensed in Ireland. Safety data from research in Europe and the US in recent years has provided reassurance that short courses of doxycycline are safe in children under 8 years of age and are not likely to produce either dental discoloration or enamel hypoplasia. This has been endorsed by the American Association of Paediatrics (AAP Red Book 2018) and Children’s Health Ireland (CHI) Group.
Sample calculation
Child requiring prophylaxis using Doxycycline 100mg unlicensed soluble tablets
Child weight=15kg (specify child weight on prescription)
Dose: 4.4mg per kg
15kg x 4.4mg/kg = 66mg dose required
How to disperse tablet to give a part dose:
Dissolve 1x 100mg soluble doxycycline tablet in 5mL of water
100mg=5mL so 66mg=3.3mL (draw up and give 3.3ml using 5ml syringe supplied by pharmacist).
For young babies use water that has been freshly boiled then cooled.
Discard remaining dose by returning to local pharmacy in child resistant closure container.
To improve palatability, can add squash/fruit juice to water. Make dose fresh each time.
Reviewed October 2021